Fibroid are the most common benign tumor of the uterus and the most common benign solid tumor in female. Histological, this tumor is composed of smooth muscle and fibrous connective tissue, so named as uterine leiomyoma, myoma or fibromyoma.1
INCIDENCE
It has been estimated that at least 20% of women at the age of 30 have got fibroid in their wombs. Fortunately, most of them (50%) remain asymptomatic. The incidence of symptomatic fibroid in hospital outpatient is about 3%. In colored races (black women), the incidence is even higher. These are more common in nulliparous or in those having one child infertility. The prevalence is highest between 35 and 45 years.1
HISTOGENESIS
Origin
The prevailing hypothesis is that it arises from the neoplastic single smooth muscle cell of the myometrium. The stimulus for initial neoplastic transformation is not known. The following are implicated: 1
Chromosomal abnormality—in about 40% of cases, there is a varying type of chromosomal abnormality, particularly the chromosome six or seven (re arrangements, deletions).1
RISK FACTORS FOR FIBROID1
| Increased risk | Reduced risk |
| Null parity or no childbirth
Obesity, increased body mass index (BMI), Polycystic ovary syndrome (PCOS) Hyper estrogenic state Black women High fat diet Family history |
Multiparity
Menopause Combined oral Contraceptives (COCs) use Smoking
|
Somatic mutations in myometrium cells may also be thecause for uncontrolled cell proliferation.
Role of polypeptide growth factors—epidermal growth factor (EGF), insulin-like growth factor-1 (IGF-1), transforming growth factor (TGF), stimulate the growth of leiomyoma either directly or via estrogen. A positive family history is often present.1
Growth1
It is predominantly an estrogen-dependent tumor. Estrogen and progesterone is incriminated as the cause. Estrogen dependency is evidenced by:
- Growth potentiality is limited during child bearing period
- Increased growth during pregnancy
- They do not occur before menarche
- Following menopause, there is often cessation of growth and there is no new growth at all
- It contains more estrogen receptors than the adjacent myometrium
- Frequent association of an ovulation
The growth potentiality is not squarely distributed amongst the fibroids which are usually multiple, some grow faster than the others. Overall, the rate of growth is slow and it takes about 3–5 years for the fibroid to grow sufficiently to be felt per abdomen (cf.—ovarian tumor grows in months). However, the fibroid grows rapidly during pregnancy or in cases where malignant changes take place. The newer low dose oral contraceptives may reduce the size.1
TYPES
Body & Cervical
Body
The fibroids are mostly located in the body of the uterus and are usually multiple.1
- Interstitial or Intramural (75%)
Initially, the fibroids are intra mural in position but subsequently, some are pushed outward or inward. Eventually, in about 70%, they persist in that position.1
- Sub peritoneal or Subserous (15%)
In this condition, the intramural fibroid is pushed outwards towards the peritoneal cavity. The fibroids are either partially or completely covered by peritoneum. When completely covered by peritoneum, it usually attains pedicle—called pedunculated sub serous fibroid. On rare occasion, the pedicle may be torn through; the fibroid gets its nourishment from the omental or mesenteric adhesions and is called ‘wandering’ or ‘parasitic’ fibroid. Sometimes, the intramural fibroid may be pushed out inbetween the layers of broad ligament and is called broad ligament fibroid (false or pseudo). Leiomyomas may cause pseudo-Meig’s syndrome.1
- Submucous (5%)
The intramural fibroid when pushed toward the uterinecavity, and is lying underneath the endometrial, it is called sub mucous fibroid. Submucous fibroid can make the uterine cavity irregular and distorted. Pedunculated sub mucous fibroid may come out through the cervix. It maybe infected or ulcerated to cause metrorrhagia. Although, this variety is least common (about 5%) but it produces maximum symptoms.1
Cervical
Cervical fibroid is rare (1–2%). In the supra vaginal part of the cervix, it may be interstitial or sub peritoneal variety and rarely polypoidal. Depending upon the position, it may be anterior, posterior, lateral or central. Interstitial growths may displace the cervix or expand it so much that the external so is difficult to recognize. All these disturb the pelvic anatomy, specially the ureter. In the vaginal cervix, the fibroid is usually pedunculated and rarely sessile.1
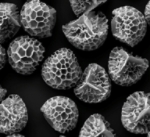
Microscopic Appearance
The tumor consists of smooth muscles and fibrous connective tissues of varying proportion. Originally, it consists of only muscle element but later on, fibrous tissues inter mingle with the muscle bundles. As such, the nomenclature of ‘fibroids’ although commonly used, is in appropriate and should better be called either myomata or fibromyomata.1
SECONDARY CHANGES IN FIBROIDS
DEGENERATIONS
- Hyaline degeneration is the most common (65%) type of degeneration affecting all sizes of fibroids except the tiny one. It is common especially in tumor shaving more connective tissues. The central part of the tumor, which is least vascular, is the common site. The feel becomes soft elastic in contrast to firm feel of the tumor. Naked eye examination on the cut surface shows irregular homogenous areas with loss of whorl-like appearance. Microscopic examination reveals hyaline changes of both the muscles and fibrous tissues.1
- Cystic degeneration usually occurs following menopause and is common in interstitial fibroids. It is formed by liquefaction of the areas with hyaline changes. Irregular ragged walls line the cystic spaces. The cystic changes of an isolated big fibroid maybe confused with an ovarian cyst or pregnancy.1
- Fatty degeneration is usually found at or after menopause. Fat globules are deposited mainly in the muscle cells.1
- Calcific degeneration (10%) usually involves the sub serous fibroids with small pedicle or myomas of postmenopausal women. It is usually preceded by fatty degeneration. There is precipitation of calcium carbonate or phosphate within the tumor. When whole of the tumor is converted into a calcified mass, it iscalled “womb stone”.1
- Red degeneration (carneous degeneration) occurs in a large fibroid mainly during second half of pregnancy and puerperium. Partial recovery is possible and as such called necrobiosis. The cause is not known but is probably vascular in origin. Infection does not play any part.1
- Atrophy: Atrophic changes occur following menopause due to loss of support from estrogen. There is reduction in the size of the tumor. Similar reduction also occurs following pregnancy enlargement.1
- Necrosis: Circulatory in adequacy may lead to central necrosis of the tumor. This is present in sub mucous polyp or pedunculated sub serous fibroid.1
- Infection: The infection gains access to the tumor core through the thinned and sloughed surface epithelium of the sub mucous fibroid. This usually happens following delivery or abortion. Intramural fibroid may also be infected following delivery.1
- Vascular changes: Dilatation of the vessels (telangiectasis) or dilatation of the lymphatic channels (lymphangiectasis) inside the myoma may occur. The cause is not known.1
- Sarcomatous changes: Sarcomatous change mayoccur in less than 0.1% cases. The usual type is leiomyosarcoma. Recurrence of fibroid polyp, sudden enlargement of fibroid or fibroid along with Postmenopausal bleeding raises the suspicion.1
Associated Changes in the Pelvic Organs
- Uterus: The shape is distorted; usually asymmetrical but at times, uniform. Myohyperplasia is almost a constant finding. It may be due to hyperestrinism or work hypertrophy in an attempt to expel the fibroid. The endometrium may be of normal type. In others, there are features of an ovulation with evidences of hyperplasia.1
There is dilatation and congestion of the myometrial and endometrial venous plexuses. The endometrium as a result becomes thick, congested, and edematous. The endometrial overlying the sub mucous fibroid may be thin and necrotic with evidences of infection. The uterine cavity may be elongated and distorted in intramural and sub mucous varieties.1
- Uterine tubes: The frequent tubal infection (about 15%) detected in association with fibroid seems coincidental.1
- Ovaries: The ovaries may be enlarged, congested, and studded with multiple cysts. The cause may be due to hyperestrinism.1
- Ureter: There may be displacement of the anatomy of the ureter in broad ligament fibroid. The compression effect results in hydro ureter and or hydro nephrosis.1
- Endometriosis: There is increased association of pelvic endometriosis and adenomyosis (30%).1
- Endometrial carcinoma: The incidence remains unaffected.1
CLINICAL FEATURES
Patient Profile
The patients are usually nulli parous or having long period of secondary infertility. However, early marriage and frequent child birth make its frequency high even amongst the multi parous women. The incidence is at its peak between 35–45 years. There is a tendency of delayed menopause.1
SYMPTOMS
The majority of fibroids remain asymptomatic (75%). They are accidentally discovered by the physician during routine examination or at laparotomy or laparoscopy. The symptoms are related to anatomic type and size of the tumor. The site is more important than the size. A small sub mucous fibroid may produce more symptoms than a big subserous fibroid.1
SYMPTOMS OF FIBROID UTERUS1
- Asymptomatic—majority (75%)
- Menstrual abnormality: Menorrhagia, metrorrhagia
- Dysmenorrhea
- Dyspareunia
- Subfertility
- Pressure symptoms
- Recurrent pregnancy loss (miscarriage, preterm labor)
- Lower abdominal or pelvic pain
- Abdominal enlargement
1) Menstrual abnormalities:
- Menorrhagia (30%) is the classic symptom ofsymptomatic fibroid.
The menstrual loss is progressively increased with successive cycles. It is conspicuous in sub mucous or interstitial fibroids.1
The causes are: 1
- Increased surface area of the endometrial (Normal is about 15 cm2)
- Interference with normal uterine contractility due to inter position of fibroid
- Congestion and dilatation of the subjacent endometrial venous plexuses caused by the obstruction of the tumor
- Endometrial hyperplasia due to hyperestrinism(an ovulation)
- Pelvic congestion
- Role of prostanoids—imbalance of thromboxane (TXA2) and prostacyclin (PGI2) with relative deficiency of TXA2.
- Metrorrhagia or irregular bleeding: 1
- Ulceration of submucous fibroid or fibroid polyp
- Torn vessels from the sloughing base of a polyp
- Associated endometrial carcinoma.
2) Dysmenorrhea: The congestive variety may be due to associated pelvic congestion or endometriosis. Spasmodic type is associated with extrusion of polyp and its expulsion from the uterine cavity. Sub serous, broad ligament or cervical fibroids are usually unassociated with menstrual abnormalities.1
3) Infertility: Infertility (30%) may be a major complaint.1
The probable known attributing factors are: 1
Uterine
- Distortion and/or elongation of the uterine cavity _difficult sperm ascent
- Preventing rhythmic uterine contraction due to fibroids during inter course _ impaired sperm transport
- Congestion and dilatation of the endometrial venous plexuses _ defective implantation
- Atrophy and ulceration of the endometrial over the sub mucous fibroids _ defective nidation
- Menorrhagia and dyspareunia.
Tubal
- Cornual block due to position of the fibroid
- Marked elongation of the tube over a big fibroid
- Associated salpingitis with tubal block.
Ovarian: _ an ovulation
Peritoneal: _ Endometriosis
Unknown—(majority)
3) Pregnancy-related problems like abortion, pre term labor and intra uterine growth restriction are high. The reasons are defective implantation of the placenta, poorly developed endometrial, reduced space for the growing fetus and placenta. Red degeneration and torsion of sub serous pedunculated fibroid is common in pregnancy. Labor dystocia, increased operative delivery postpartum hemorrhages are also more.1
4) Pain lower abdomen1
The fibroids are usually painless. Pain may be due to some complications of the tumor or due to associated pelvic pathology.
- Due to tumor
-Degeneration
-Torsion subserous pedunculated fibroid
– Extrusion of polyp
- Associated pathology
– Endometriosis
– Pelvic inflammatory disease (PID).
5) Abdominal swellings (lump)
The patient may have a sense of heaviness in lower abdomen. She may feel a lump in the lower abdomen even without any other symptom.1
6) Pressure symptoms
Pressure symptoms are rare in body fibroids. The fibroids in the posterior wall may be impacted in the pelvis producing constipation; dysuria or even retention of urine. A broad ligament fibroid may produce ureteric compression_ hydroureteric and hydronephrotic changes _ infection_ pyelitis.1
SIGNS1
General examination reveals varying degrees of pallor depending upon the magnitude and duration of menstrual loss.
Abdominal examination
The tumor may not be sufficiently enlarged to be felt per abdomen. But if enlarged to 14 weeks or more, the following features are noted:
Palpation
- Feel is firm, more toward hard; may be cystic in cystic degeneration
- Margins are well-defined except the lower pole which cannot be reached suggestive of pelvic in origin
- Surface is nodular; may be uniformly enlarged in a single fibroid
- Mobility is restricted from above downwards but can be moved from side to side.
Percussion
The swelling is dull on percussion.
Pelvic examination
Bimanual examination reveals the uterus irregularly enlarged by the swelling felt per abdomen, the swelling in uterine is evidenced by:
- Uterus is not felt separated from the swelling and as such a groove is not felt between the uterus and the mass.
- The cervix moves with the movement of the tumor felt per abdomen.
The only exception of these two findings is a sub serous pedunculated fibroid. As such, such type is too often confused with an ovarian tumor. However, a sub mucous fibroid may produce symmetrical enlargement of the uterus and at times, it is difficult to diagnose accurately.1
COMPLICATIONS OF FIBROIDS1
|
INVESTIGATIONS1
The investigations aim at:
- To confirm the diagnosis
- Pre operative assessment
To Confirm the Diagnosis1
Although, the majority of uterine fibroids can be diagnosed from the history and pelvic examination but at times pose problems in diagnosis.
- Ultrasound and Color Doppler (TVS) findings—1
(i) Uterine contour is enlarged and distorted;
(ii) Depending on the amount of connective tissue or smooth muscle proliferation, fibroids are of different echogenecity – hypo echoic or hyper echoic;
(iii) Vascularization is at the periphery of the fibroid and
(iv) Central vascularization indicates degenerative changes.
Ultrasound is a useful diagnostic tool to confirm the diagnosis of fibroid. Transvaginal ultrasound can accurately assess the myoma location, dimensions volume and also any adnexal pathology. Hydro ureter or hydro nephrotic changes can be diagnosed. Three-dimensional ultrasonography can locate fibroids accurately. Serial ultrasound examination is needed during medical or conservative management1
- Saline Infusion Sonography (SIS) is helpful to detect any sub mucous fibroid or polyp.1
- Magnetic resonance imaging (MRI)—is more accurate compared to ultrasound. It helps to differentiate adenomyosis from fibroids. MRI is not used routinely for the diagnosis. It is expensive and not widely available.1
- Laparoscopy—Laparoscopy is helpful, if the uterine size is less than 12 weeks and associated with pelvic pain and infertility. Associated pelvic endometriosis and tubal pathology can be revealed. It can also differentiate a pedunculated fibroid from ovarian tumor, not revealed by clinical examination and ultrasound.1
- Hysteroscopy is of help to detect sub mucous fibroid in unexplained infertility and repeated pregnancy wastage.The presence and site of sub mucous fibroid can be diagnosed by direct visualization during hysteroscopy. Submucosal fibroid can be resected at the same time using a resecting hysteroscope.1
- HSG when done, a filling defect can be seen.1
- Uterine curettage—In the presence of irregular bleeding, to detect any coexisting pathology and to study the endometrial pattern, curettage is helpful. It additionally helps to diagnose a sub mucous fibroid by feeling a bump. However, hysteroscopy and biopsy is a better alternative.1
Preoperative Assessment
Apart from routine preoperative investigations, intravenous pyelography to note the anatomic changes of the ureter may be helpful.1
DIFFERENTIAL DIAGNOSIS1
The fibroid of varying sizes may be confused with:
(1) Pregnancy (2) Full bladder (3) Adenomyosis (4) Myohyperplasia (5) Ovarian tumor (6) Tubo-Ovarian mass.
MANAGEMENT OF FIBROID UTERUS1
- ASYMPTOMATIC MANAGEMENT (75%)
Fibroids detected accidentally on routine examination for complaints other than fibroids are dealt with as follows:
– Observation: A certain diagnosis of fibroid should be a must, prior to contemplating expectant management. The risk of sarcomatous changes is so insignificant (0.1%) that prophylactic removal of fibroid is unjustified in asymptomatic cases.1
–Indications of expectant management:
- Size <12 weeks (of pregnancy size)
- Diagnosis certain
- Follow up possible.
Periodic examination at interval of 6 months andultrasound evaluation annually is needed. If the symptomsof fibroid appear and or it grows and increases in size, surgery is indicated as per conventional therapy.1
- SYMPTOMATIC MANAGEMENT
Medical Management
Homeopathic medicines can be used for the management of symptomatic fibroids. The medicines used are either as a temporary palliation or may be used to reduce the size of fibroid. This needs to be planned based on symptom severity, age of patient, location of fibroid and related factors.1
Preoperative therapy: It is indeed advantageous to reduce the size and vascularity of fibroid prior to either myomectomy or hysterectomy. While operation will be technically easier in broad ligament or cervical fibroid, in myomectomy, there may be little difficulty in enucleation of the tumor from its pseudo capsule. Benefits are achieved when therapy is given for a period of three to six months.1
Surgical Management of Fibroid Uterus1
- Myomectomy
(May be done by)
- Laparotomy
- Laparoscopy
- Hysteroscopy
Embolotherapy
Laparoscopic uterine artery ligation
Myolysis
Endometrial ablation
Hysterectomy
Endoscopic Surgery
FOLLOWING ARE DO’S AND DON’TS
Do’s –
- Fruits and Vegetables – Intake of plenty of fruits like apples and tomatoes, and vegetables like broccoli and cabbage, could lower the risk of developing fibroids.
- Blood pressure – Managing blood pressure, either with diet, life style, or medication helps in reducing symptom of fibroids.
- Stress level –There is a great impact of stress on fibroid. Doing yoga, massage, and exercise help managing stress. Acupuncture also can help relieve period pain.
- Pain during menses/ periods – Lying down and elevating legs with a pillow. Or lie on your side and bring kneesinto your chest to take the pressure off your back helps in painful periods due to fibroids.
- Be regular with your workouts – Women exercising the most (about 7 hours per week of activities like running, dancing, or walking) had the lowest chance of developing fibroids. Exercise can also help keep your blood pressure down.
Don’ts –
- Avoid processed foods, red meats, and high-fat dairy – These foods, alcohol and caffeine can make fibroids worse.
- Don’t skip your workouts –
- Don’t overdo it on the sugar – Eating a high-sugar diet could be linked to a higher risk of fibroids.
- Don’t smoke – Smoking can increase your period pain because it reduces the amount of oxygen that gets to your pelvic region.
SCOPE OF HOMEOPATHY
Medicines need to be taken under the guidance of an expert homeopath. All symptomatic women need treatment. The treatment depends upon the age of the patient, need for preserving reproductive functions, severity of the symptoms, extent of the disease, and the attitude of the patient towards her problem. The objective of the treatment should be to first to help alleviate symptoms and then reduce the size of the fibroid. Facilitate child bearing and enable the patient to lead a comfortable life. Therefore, the treatment should be individualized.
There are many medicines in homeopathic literature which indicates its usage for uterine fibroids. A well selected homeopathic remedy and one based on pathological action of remedy can help treat this condition. Many acute medicines are available to help in symptoms due to fibroids. The second intent of treatment is to stop the growth of fibroid and then reduce the size of fibroid. Females where fibroids are detected near menopause, there symptomatic management is the main intent and once menses stop the fibroids start shrinking on their own. A regular check up post menopause shall be done to check the fibroids which usually remain uneventful once menopause is there.
SOME MEDICINES USEFUL FOR UTERINE FIBROID
 Calcarea carbonica
Calcarea carbonica
Premature, profuse and protracted (atony of muscular coat of uterus and relaxation) the LEAST EXCITEMENT CAUSES RETURN OF MENSES; monthly sickness during lactation; discharge light- colored or bright red. Before; nervousness, nocturnal shivering and colicky pains; aching pain in back and hips: sensitiveness and swelling of mammae (Lac.can,); during. Complications of uterine and chest affections.2
 Hydrastis Canadensis
Hydrastis Canadensis
Uterine catarrh, endometritis, with mucopurulent, stringy discharge and great debility. For epithelial abrasion of cervix, os and vagina apply locally, one ounce in hot water.2
 Lycopodium clavatum
Lycopodium clavatum
Menses too profuse and of too long duration, inclined to be late, with great sadness before periods. Ovaries diseased, right to left, ovarian tumors. Dry, pediculated, painless condylomata.2
 Mercurius Solubilis
Mercurius Solubilis
Menses too profuse attended with colic and much anxiety.2
 Phosphorous
Phosphorous
Menses too early and too scanty, from 2 to 8 days. Hemorrhage from the uterus. Hemorrhages become more and severe often so severe that anemia is the consequence.2
 Sabina
Sabina
Menses profuse, bright. Uterine pains extend to the thighs. Discharge of blood between the periods. Menorrhagia. Inflammation of ovaries and uterus after abortion. Pain from sacrum to pubis. Hemorrhage partly clotted.2
 Silicea Terra
Silicea Terra
Menses are very irregular every 2 or 3 months. Discharge of white water from the uterus instead of menses. Tendency to growths and tumors.2
References
- Dutta DC, Textbook of Gynecology. 7threv.ed. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd.; 2016.
- 568p.Boericke W. New Manual of Homœopathic Materia Medica and Repertory. 9th Reprinted Edition. New Delhi: B Jain Publishers (P) Ltd; 2005.
