 Cystitis – Scope of Homeopathy
Cystitis – Scope of Homeopathy
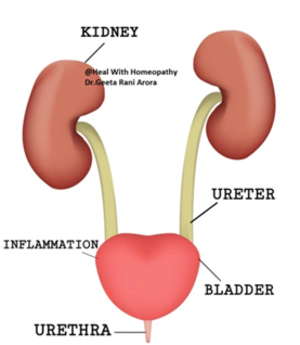
In health, the upper urinary tract it sterile but the lower urinary tract there are bacteria which thrive in lower urinary tract. The urinary tract can become infected with various bacteria but the most common is E. coli derived from the gastrointestinal tract. The most common presenting problem is cystitis with urethritis (generally referred to as urinary tract infection).1
Urinary tract infection (UTI) is the term used to describe acute urethritis and cystitis caused by a microorganism. It is a common disorder, accounting for 1–3% of consultations in general medical practice. The prevalence of UTI in women is about 3% at the age of 20, increasing by about 1% in each subsequent decade. In males, UTI is uncommon, except in the first year of life and in men over 60, when it may complicate bladder outflow obstruction.1
Pathophysiology1
Urine is an excellent culture medium for bacteria; in addition, the urothelium of susceptible persons may have more receptors, to which virulent strains of E. coli become adherent. In women, the ascent of organisms into the bladder is easier than in men; the urethra is shorter and the absence of bactericidal prostatic secretions may be relevant. Sexual intercourse may cause minor urethral trauma and transfer bacteria from the perineum into the bladder. Instrumentation of the bladder may also introduce organisms. Multiplication of organisms then depends on a numberof factors, including the size of the inoculum and virulence of the bacteria. Conditions that predispose to UTI.1
Clinical features1
Typical features of cystitis and urethritis include:
- Abrupt onset of frequency of micturition and urgency.
- Burning pain in the urethra during micturition (dysuria).
- Suprapubic pain during and after voiding.
- Intense desire to pass more urine after micturition, due to spasm of the inflamed bladder wall (strangury).
- Urine that may appear cloudy and have an unpleasant odour.
- Non-visible or visible haematuria.
Systemic symptoms are usually slight or absent. However, infection in the lower urinary tract can spread to cause acute pyelonephritis (inflammation of a part of the kidneys). This is suggested by prominent systemic symptoms with fever, rigors, vomiting, hypotension and loin pain, guarding or tenderness, and may be an indication for hospitalisation. It is important to note that only about 30% of patients with acute pyelonephritis have associated symptoms of cystitis or urethritis. Prostatitis is suggested by perineal or suprapubic pain, pain on ejaculation and prostatic tenderness on rectal examination. The differential diagnosis of lower urinary tract symptoms includes urethritis due to sexually transmitted disease, notably chlamydia and urethritis associated with reactive arthritis. Some patients, usually female, have symptoms suggestive of urethritis and cystitis but no bacteria are cultured from the urine (the ‘urethral syndrome’). Possible explanations include infection with organisms not readily cultured by ordinarymethods (such as Chlamydia and certain anaerobes), intermittent or low-count bacteriuria, reaction to toiletries or disinfectants, symptoms related to sexual intercourse, or post-menopausal atrophic vaginitis.1
When a UTI is suspected, it can be classified into three types: 2
- Asymptomatic bacteriuriais diagnosed when a screening urine culture performedfor a reason unrelated to the genitourinary tract is incidentally found to contain bacteria, but the pt has no local or systemic symptoms referable to the urinary tract.
- Cystitis presents as dysuria, urinary frequency, and urgency; nocturia, hesitancy, suprapubic discomfort, and gross hematuria are often noted as well. Unilateral backor flank pain and fever are signs that the upper urinary tract is involved.
- Pyelonephritis presents as fever, lower-back or cost vertebral-angle pain, nausea, and vomiting. Bacteremia develops in 20–30% of cases.
– Papillary necrosis can occur in pts with obstruction, diabetes, sickle cell disease,or analgesic nephropathy.
– Emphysematous pyelonephritis is particularly severe, is associated with the production of gas in renal and perinephric tissues, and occurs almost exclusively in diabetic pts.
– Xanthogranulomatous pyelonephritis occurs when chronic urinary obstruction(often by staghorn calculi), together with chronic infection, leads to supportive destruction of renal tissue.
- Prostatitis can is either infectious or noninfectious; noninfectious cases are farmore common. Acute bacterial prostatitis presents as dysuria, urinary frequency, fever, chills, symptoms of bladder outlet obstruction, and pain in the prostatic, pelvic, or perineal area.
 Complicated UTI presents as symptomatic disease in a man or woman with an anatomic predisposition to infection, with a foreign body in the urinary tract, or withfactors predisposing to a delayed response to therapy.2
Complicated UTI presents as symptomatic disease in a man or woman with an anatomic predisposition to infection, with a foreign body in the urinary tract, or withfactors predisposing to a delayed response to therapy.2
Investigations1
In a healthy woman with a single lower urinary tract infection, urine culture prior to treatment is not mandatory. Investigation is necessary, however, in patients with recurrent infection or after failure of initial treatment, during pregnancy, or in patients susceptible to serious infection, such as the immune compromised those with diabetes or an in dwelling catheter, and older people. The diagnosis can be made from the combination of typical clinical features and abnormalities on urinalysis. Most urinary pathogens can reduce nitrate to nitrite, and neutrophils and nitrites can usually be detected in symptomatic infections by urine dipstick tests for leucocyte esterase and nitrite, respectively. The absence of both nitrites and leucocyte esterase in the urine makes UTI unlikely. Interpretation of bacterial counts in the urine, and of what is a ‘significant’ culture result, is based on probabilities. Urine taken by suprapubic aspiration should be sterile, so the presence of any organisms is significant. If the patient has symptoms and there are neutrophils in the urine, a small number of organisms is significant. In asymptomatic patients, more than 105 organisms/ml is usually regarded as significant (asymptomatic bacteriuria).1
Typical organisms causing UTI in the community include E. coli derived from the gastrointestinal tract (about 75% of infections), Proteus spp., Pseudomonas spp., streptococci and Staphylococcus epidermidis.1
Investigations to detect underlying predisposing factors for UTI are used selectively, most commonly in children, men or patients with recurrent infections.1
Investigation of patients with urinary tract infection1
All patients
Dipstick* estimation of nitrite, leucocyte esterase and glucose
Microscopy/cytometry of urine for white blood cells, organisms
Urine culture
Infants, children, and anyone with fever or complicated infection
Full blood count; urea, electrolytes, creatinine
Blood cultures
Pyelonephritis: men; children; women with recurrent infections
Renal tract ultrasound or CT
Pelvic examination in women, rectal examination in men
Continuing haematuria or other suspicion of bladder lesion
Cystoscopy
Urinary infection in old age1
Prevalence of asymptomatic bacteriuria: Rises with age. Among the frailest in institutional care it rises to 40% in women and 30% in men.
Decision to treat: Treating asymptomatic bacteriuria does not improve chronic incontinence or decrease mortality or morbidity from symptomatic urinary infection. It risks adverse effects from the antibiotic and promotion of the emergence of resistant organisms. Bacteriuria should not be treated in the absence of urinary symptoms.
Source of infection: The urinary tract is the most frequent source of bacteraemia in older patients admitted to hospital.
Incontinence: New or increased incontinence is a common presentation of UTI in older women.
Treatment: post-menopausal women with acute lower urinary tract symptoms may require longer than 3 days’ therapy.
Risk factors for urinary tract infection1
Bladder outflow obstruction
Benign prostatic enlargement
Prostate cancer
Urethral stricture
Anatomical abnormalities
Vesico-ureteric reflux
Uterine prolapse
Bladder fistula
Neurological problems
Multiple sclerosis
Spina bifida
Diabetic neuropathy
Foreign bodies
Urethral suprapubic catheter
Ureteric stent
Nephrostomy tube
Urolithiasis
Loss of host defences
Atrophic urethritis and vaginitis in post-menopausal women
Diabetes mellitus
Management1
For infection of the lower urinary tract, in conventional therapy treatment for 3 days is the norm and is less likely to induce significant alterations in bowel flora than more prolonged therapy. Relevant antibiotics are used which are used as the usual first choice of drug for initial treatment; however, between 10% and 40% of organisms causing UTI are resistant to first line antibiotics, the lower rates being seen in community-based practice. Then, higher grade antibiotics need to be used. They may be used once cultures confirm that the organism is sensitive. The safety of antibiotics for children and pregnancy has to be looked into, so it’s imperative to consult a physician and do not do self-prescription.
In more severe infection, antibiotics usage is longer. A fluid intake of at least 2 L/day is usually recommended, although this is not based on evidence and may make symptoms of dysuria worse.
Homeopathic Management of Cystitis
Homeopathic medicines are helpful for acute as well as chronic cystitis. There are few medicines like Apis mellifica, Cantharis and Apocyanum which are very good for acute infections. There are few medicines which are mainly known for mild cystitis or chronic cases. Some are detailed below. Contact your homeopathic practitioner for right selection of medicines.
 Apis mellifica
Apis mellifica
Great irritation at neck of bladder, with frequent and burning irritation, repeated micturition every few minutes all day; scalding sensation and soreness when urinating; burning and stinging in urethra; difficult urination in children; incontinence, with great irritation of the parts, urine red, hot, bloody and scanty. 5
 Asparagus officinalis
Asparagus officinalis
Its marked and immediate action on the urinary secretion is well known. [2] Frequent, with fine stitches in orifice of urethra; burning; of peculiar odor. [2]
Cystitis, with pus, mucus and tenesmus. [2]Lithiasis.
Frequent and distressing tenesmus, urine loaded with pus and flakes of the mucous lining of the bladder; constant urging to urinate; burning in urethra during and after micturition.5
 Belladonna
Belladonna
Cystitis, inflammation of bladder Sensation of turning and twisting in bladder, like a large worm, without desire to urinate; vesical region very sensitive to the least jar; urine hot and fiery red, clear at first, but soon becoming turbid on standing and depositing a copious, slimy, bright-red, bran like sediment; urine passed in drops with frequent urging. 5
 Berberis vulgaris
Berberis vulgaris
Pain in region of kidneys is most marked; hence its use in renal and vesical troubles, and vesical catarrh. [2]
Sensation as if some urine remained after urinating. Urine with thick mucus and bright-red, mealy sediment. Bubbling, sore sensation in kidneys. Pain in bladder region. Pain in the thighs and loins on urinating. Frequent urination; urethra burns when not urinating. [2]
Cutting in bladder extending down urethra, burning pain even after urinating, urine yellow, turbid and flocculent; back lame and sore with pain in loins and hips.5
Cantharis vesicatoria
Constant urging to urinate, passing but a few drops at a time, which is mixed with blood (sudden desire to urinate and intense itching in urethra, Petros.).3
Cystitis, inflammation of bladder Violent tenesmus vesicae and strangury; violent burning, cutting pains in neck of bladder, extending to fossa navicularis; violent pains in bladder, urging to urinate from smallest quantity of urine; painful discharge of a few drops of bloody urine, causing very sharp pain, as if a red-hot iron were passed along urethra.3
 Chimaphila umbellate
Chimaphila umbellate
Acts principally on kidneys, and genito-urinary tract; affects also lymphatic and mesenteric glands and female mammae. [2]
Plethoric young women with dysuria. 2
One of the remedies whose symptoms point to its employment in bladder affections, notably catarrh, acute and chronic. [2]
Burning and scalding during micturition, and straining afterwards. [2]
Must strain before flow comes. [2]
Unable to urinate without standing with feet wide apart and body inclined forward. [2]
 Copaiva officinalis
Copaiva officinalis
Acts powerfully on mucous membranes, especially that of the urinary tract, the respiratory organs, and the skin, here producing a well-marked nettle-rash. [2]
Burning in neck of bladder and urethra; pressure on bladder, with frequent ineffectual urging and passing the urine by drops; frothy, dark-yellow urine with the odor of violets; swelling and dilatation of orifice of urethra. 5
Retention, with pain in bladder, anus, and rectum. [2]
Constant desire to urinate. [2]
 Cubeba officinalis
Cubeba officinalis
Cystitis, inflammation of bladder Chronic cystitis; cutting and constriction after micturition; with sensation as if the bladder still contained water; last drops of urine passed with pain; urine foamy, bloody, smells of violets; haematuria.5
Frequent urination of a nervous origin. [2]
Urethritis, with much mucus, especially in women. [2]
Cutting after urination, with constriction. [2]
Haematuria. [2]
Prostatitis, with thick yellow discharge. [2]
 Equisetum hyemale
Equisetum hyemale
Principal action on the bladder. [2]A remedy for enuresis and dysuria.4
Cystitis, inflammation of bladder Severe and dull pain in bladder, not abating after urination, with tenderness on pressure and soreness of testicles and cords; excessive burning or sharp cutting pains in urethra; great desire to micturate, but only a small amount passed each time; urine high-colored and scanty; great irritability of the bladder with pains through hips and thighs.5
 Lycopodium clavatum
Lycopodium clavatum
Chronic cases, strangury, stitches simultaneously in anus and neck of bladder; heaviness and dull pressure in bladder; frequent urging, forcing patient to retain the urine and to support abdomen with both hands; urging, but must wait a long time before urine passes; emission delayed, with pain in back, amel. Soon after flow begins. Red sand in urine, on child’s diaper (Phos.); child cries before urinating (Bor.); pain in back, relieved by urinating; renal colic, right side (left side, Berb.).1 Pains: aching-pressure, drawing; chiefly right-sided, < four to eight p.m. [1] pain aggr. On lying down, especially at night; amel. By horseback riding.5
 Polygonum hydropiperoides
Polygonum hydropiperoides
Painful constriction at neck of bladder.4Cystitis, inflammation of bladder – cutting and feeling of strangulation at the neck of bladder when urinating, lasting a long time; pains in sacrum and bladder, with a desire to micturate, not relieved by voiding large quantities of urine. 5
 Sarsaparilla officinalis
Sarsaparilla officinalis
Urine scanty, slimy, flaky, sandy, bloody. Severe pain at conclusion of urination. Urine dribbles while. Bladder distended and tender.4Chronic cystitis; frequent, inefficient urging to urinate and diminished excretion; severe tenesmus as in gravel, with emission of white, acrid, turbid matter and mucus; much pain at the conclusion of passing water; during micturition air passes from the bladder; sand in urine, the child screams before and while passing it; urine irritating, bright and clear, or scanty, flaky with deposit of sand; intolerable smell of the genitals.5
 Solidago virgaurea
Solidago virgaurea
Urine – Scanty, reddish brown, thick sediment, dysuria, gravel. Difficult and scanty. Albumen, blood, and slime in urine. Pain in kidneys extends forward to abdomen and bladder. [Berb.] Clear and offensive urine.4 sometimes makes the use of the catheter unnecessary. 4
 Terebinthinae oleum
Terebinthinae oleum
Strangury, with bloody urine.4 Urethritis, with painful erections. [Canthar.] 4 Constant tenesmus.4 Haematuria: blood thoroughly mixed with the urine; sediment, like coffee-grounds; cloudy, smoky, albuminous; profuse, dark or black, painless.3 Violent burning and cutting in bladder; tenesmus; sensitive hypogastrium; cystitis and retention from atony of fundus.3 Urine rich in albumin and blood, but few if any casts; < from living in damp dwellings.3 Urine retained at the fundus of the bladder from atony in old persons of a sedentary habit. 5
 Uvaursi
Uvaursi
Dysuria, strangury; frequent urging with little discharge, followed by burning, cutting pains; has to lie on his back to pass urine; profuse mucous sediment, very tenacious, passed with great straining; severe spasm in bladder before micturition; constipation..5Urinary symptoms most important.2 Cystitis, with bloody urine.4Chronic vesical irritation, with pain, tenesmus, and catarrhal discharges. 4
Dietary Recommendations for Cystitis: 6
 Some beneficial natural foods:
Some beneficial natural foods:
- Cranberry juice contains phytonnutrients that seem to prevent bacterial infections of urinary tract. This action may reduce or prevent the symptoms of cystitis. A daily 300ml glass of cranberry juice is estimated to be sufficient to prevent Escherichia coli attachment.
- Blueberries contain similar phytonutrients and appear to be effective in fighting this bacterium.
- Celery cleanses uric acid from the system. An infusion taken three times a day may help.
- Garlic has natural antibiotic properties and is worth eating regularly to help fight infections.
- Dandelion leaf tea and dandelion extract are diuretics that can help to cleanse the system.
- Bearberry is known for its antiseptic properties: This herb can be made into an infusion by simmering 15g of the leaves with 500ml of water
 Food items to be avoided:6
Food items to be avoided:6
- Coffee, tea, cola, and cold remedies contain caffeine, which makes bladder irritation worse.
- Citrus fruits, spicy foods, tomatoes, alcohol, and chocolate may make symptoms worse.
Other Dietary Measures:
- Try and drink about 300ml of water every 20 minutes or so in order to flush out the system.
- You can use: Bicarbonate of soda dissolved in 30Oml of water twice daily reduces the acidity of the urine. Make sure u is not allergic to it. The taste can be disguised with fruit juice.
References
- Ralston S.H., Penman I.D., Strachan M.W.J., Hobson R.P. Davidson’s, Principles and Practice of Medicine. 23rdrev.ed. Edinburgh; Churchill Livingstone/Elsevier; 2018. 1417p.
- Kasper D.L., Fauci A.S., Hauser S.L., Longo D.L., Jameson J.L., Loscalzo J. Harrison’s Manual of Medicine. 19th rev. ed.United States: McGraw Hill; 2016, 1222p.
- ALLEN H. C., Keynotes and Characteristics with Comparisons
- BOERICKE W., Pocket Manual of Homeopathic Materia Medica
- LILIENTHAL S., Homoeopathic Therapeutics
- AMANDA URSELL., The Complete Guide Healing Foods
